What Is Peripheral Neuropathy?
Peripheral neuropathy describes any condition that damages the peripheral nerves, which are responsible for transmitting sensory and motor information between the central nervous system (brain and spinal cord) and the rest of the body. These nerves include three main types: sensory fibres that convey sensations like touch and temperature; motor fibres that control muscle movements; and autonomic fibres that regulate involuntary functions such as heart rate, digestion, and blood pressure.
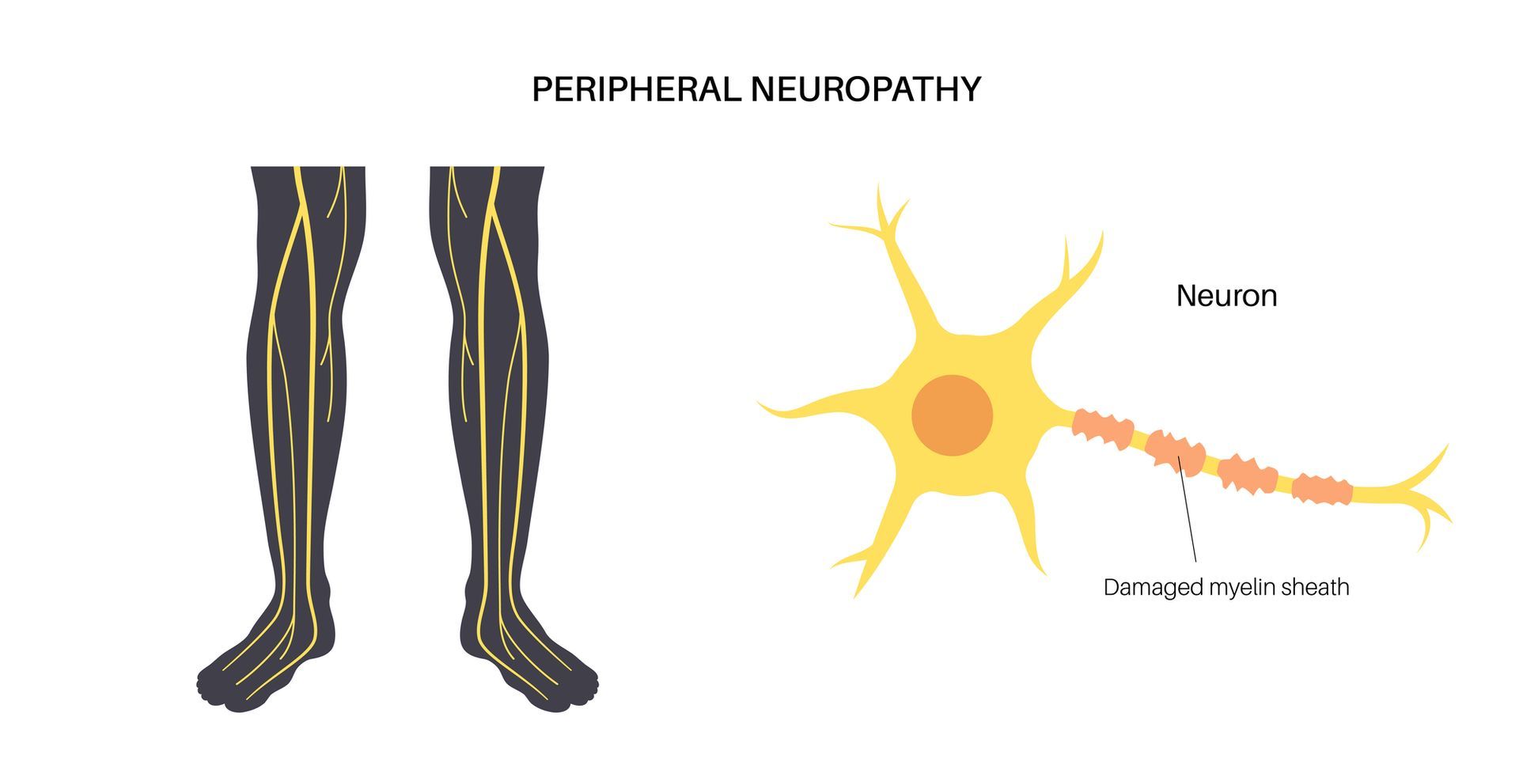
Damage can occur to a single nerve (mononeuropathy), multiple individual nerves (multiplex neuropathy), or many nerves simultaneously (polyneuropathy). Common abnormalities involve axonal degeneration, demyelination (loss of the nerve’s insulating sheath), or a combination of both, ultimately disrupting nerve signal transmission and leading to a spectrum of clinical symptoms.
Types of Peripheral Neuropathy
Peripheral neuropathies are often classified by the primary type of nerve fibres affected:
Sensory Neuropathy
Sensory neuropathy impairs the nerves that convey sensations, leading to symptoms such as numbness, tingling (“pins and needles”), and burning pain, often beginning in the feet and hands and progressively moving inward.
Motor Neuropathy
Motor neuropathy affects the nerves responsible for muscle control, resulting in muscle weakness, cramps, twitching, and difficulties with coordination and balance.
Autonomic Neuropathy
Autonomic neuropathy targets the nerves that regulate involuntary bodily functions, causing issues such as orthostatic hypotension (dizziness or fainting when standing), gastrointestinal disturbances (constipation, diarrhea, gastroparesis), urinary problems (bladder dysfunction), and abnormal sweating.
Small Fibre Neuropathy
Small fibre neuropathy predominantly damages small sensory fibres, producing sharp, burning pain and temperature sensitivity in the extremities, and can be confirmed via specialized nerve tests and skin biopsies.
Mononeuropathy
Mononeuropathy involves damage to a single peripheral nerve—often due to trauma, compression (e.g., carpal tunnel syndrome), or localized injury—presenting as focal pain, weakness, or numbness in the affected area.
Causes and Risk Factors
While peripheral neuropathy can stem from a multitude of sources, key contributors include:
Diabetes Mellitus
Diabetes accounts for over half of all cases of peripheral neuropathy. Chronically high blood sugar levels damage nerve fibres and their blood supply, especially in the feet and legs.
Autoimmune and Inflammatory Disorders
Conditions such as rheumatoid arthritis, lupus, and Guillain-Barré syndrome can trigger immune-mediated attacks on peripheral nerves.
Toxins and Medications
Excessive alcohol consumption, exposure to heavy metals, certain chemotherapy agents, and other neurotoxic substances can injure nerves and lead to neuropathy.
Infections
Viral or bacterial infections, including HIV, Lyme disease, and hepatitis C, can directly harm nerve tissue or induce immune responses that damage nerves.
Genetic Mutations
Inherited neuropathies such as Charcot-Marie-Tooth disease result from genetic defects that disrupt normal nerve structure or function.
Metabolic and Nutritional Factors
Kidney and liver dysfunction, vitamin deficiencies (particularly B₁₂), and metabolic disorders can impair nerve health over time.
Symptoms of Peripheral Neuropathy
Symptoms vary significantly depending on nerve type, location, and severity:
Sensory Symptoms
Patients often report numbness, tingling, burning pain, hypersensitivity to touch, and loss of proprioception (sense of position), particularly in a “stocking-and-glove” distribution.
Motor Symptoms
Muscle weakness, cramps, fasciculations (twitching), and gait disturbances may develop as motor fibres deteriorate.
Autonomic Symptoms
Dysfunction of autonomic fibres can produce dizziness or fainting upon standing (orthostatic hypotension), gastrointestinal problems (constipation, diarrhea, bloating), bladder control issues, and abnormal sweating patterns.
Symptoms typically develop gradually over months to years but can present acutely in some cases (e.g., toxin exposure or autoimmune neuropathy).
Diagnosis and Assessment
A thorough evaluation is essential to identify the type, cause, and extent of neuropathy:
1. Clinical History and Physical Examination
A healthcare provider will review symptom onset, progression, medical history, and conduct a detailed neurological exam assessing sensation, muscle strength, reflexes, and coordination.
2. Electrodiagnostic Testing
a. Nerve Conduction Studies (NCS) measure how quickly electrical impulses travel through peripheral nerves, helping detect demyelinating versus axonal neuropathies.
b. Electromyography (EMG) evaluates electrical activity in muscles, distinguishing nerve disorders from muscle diseases.
3. Laboratory Tests
Blood tests can reveal diabetes, vitamin deficiencies, kidney or liver dysfunction, autoimmune markers, and infectious agents.
4. Specialized Tests
Depending on the suspected cause, providers may order skin biopsies for small fibre neuropathy, nerve ultrasound, MRI, genetic testing, or autonomic function tests.
Treatment and Management
While some neuropathies (e.g., diabetic) cannot be fully reversed, interventions can alleviate symptoms and halt progression:
Address Underlying Conditions
Optimizing blood sugar in diabetes, treating autoimmune diseases, and discontinuing neurotoxic medications are foundational steps.
Pharmacologic Pain Management
First-line agents include anticonvulsants (e.g., gabapentin, pregabalin), certain antidepressants (e.g., duloxetine, amitriptyline), topical treatments (capsaicin, lidocaine), and analgesics tailored to individual needs.
Nutritional and Lifestyle Modifications
Supplementing deficiencies (e.g., B₁₂, alpha-lipoic acid), reducing alcohol intake, engaging in regular low-impact exercise, and maintaining a balanced diet support nerve health and may reduce pain.
Physical and Occupational Therapy
Exercises, balance training, and adaptive techniques can improve mobility, reduce fall risk, and enhance daily functioning.
Neuromodulation and Interventional Approaches
In refractory cases, therapies such as nerve blocks, electrical nerve stimulation (TENS), or spinal cord stimulators may be considered.
Living with Peripheral Neuropathy
Managing peripheral neuropathy is an ongoing process that combines medical care with self-management strategies:
Foot and Skin Care
Regular inspection for cuts, blisters, or infections—especially in those with sensory loss—prevents complications.
Assistive Devices
Orthotics, braces, or walking aids can support weakened limbs and improve safety.
Support Networks
Connecting with patient groups or counselling services can help address the emotional impact of chronic pain and disability.
Regular Monitoring
Routine check‑ups allow for adjustment of treatments, monitoring of nerve function, and early detection of complications.
Moving Forward: Taking Control of Your Nerve Health
Peripheral neuropathy is a complex, multifactorial disorder that can significantly affect quality of life. By understanding its diverse causes, recognizing early symptoms, and pursuing a comprehensive diagnostic workup, patients and healthcare providers can collaborate on personalized treatment plans. Although many neuropathies are chronic, a combination of medical therapies, lifestyle changes, and supportive interventions can greatly reduce pain, maintain function, and improve overall well‑being.
Book an assessment today to take the next step!


